Dr Ingold’s legacy ensured that we didn’t get many ‘waste-of-time’ calls overnight. Other GPs reported that they had patients ringing in the early hours to say they couldn’t sleep “so could you bring a sleeping tablet over?” or that they’d been woken by calls from patients saying they’d run out of their contraceptive pill.
The BMA reckoned that GPs were paid roughly 50p an hour for night/weekend cover at that time so there was widespread dissatisfaction. The worst I experienced was a chap who rang me at 4am to tell me he’d had a belly ache which had gone away.
The worry was that you’d get a call that sounded trivial … but wasn’t. Late one night I was rung by a nice woman who wanted to tell me that her husband had come home from the pub … and he’d got a headache. Fortunately I didn’t go into the “take a couple of paracetamols” routine. On questioning it was apparent that he hadn’t had any alcoholic drinks as he was the designated driver … and that he’d never before had a headache – and that this headache was very, very, bad. That was enough to ring alarm bells so I saw him straight away and, sure enough, the signs of a subarachnoid haemorrhage (a medical emergency requiring immediate attention) were present. I sent him straight in, he had surgery and made a good recovery. He showed his gratitude by keeping me in custard creams for the following three decades.
Another “near miss” occurred early one morning when I was called by a receptionist while I was in the shower. I can’t remember how I greeted her but I doubt if my turn of phrase was that expected of a ‘caring professional.’ She’d had a call from a mother whose child had a temperature. Bear in mind that this was in the ‘pill for every ill’ era and many parents still thought any child with a temperature couldn’t be taken out of the house but, rather, they needed antibiotics to be administered at home … so calls like this were common.
It didn’t strike me a very urgent and I was scheduled to start my morning surgery … but, before I could decide how best to handle it, the receptionist said: “While I was talking to her I could hear her son crying in the background and it sounded really weird.” That was enough to ring alarm bells. I threw on some clothes, dashed round, and injected the penicillin whilst Mum called the ambulance. It was, of course, meningococcal meningitis, and that receptionist (Jan) saved the boy’s life. He was whisked off to St John’s where he made a rapid recovery.
After about 3 months of practicing at home, the lovely Mrs Govani, who had heard of our plight, offered us the floor above her pharmacy in the town centre. This was good timing as the baby’s head was engaged at this stage so Sue couldn’t endlessly run up and down the stairs at home. We jumped at the chance and, after a basic make-over, we started working there.
It wasn’t long before we were joined by the late great Dr Praful. There were only two consulting rooms so, with a nurse &/or a midwife also present, we often ended up seeing patients in the loo/bathroom.
I ran into one nice lady comparatively recently who reminded me that, years ago, she saw me in the bathroom after she had been checked over by the midwife. It was her first pregnancy so we had a long chat. She told me that at the end of it I said: “And now it’s time for your bath” … giving her the impression that it was part of the routine. It took her a full minute and several blushes to realise that I was joking. I still feel guilty about that!
One day I was working in the furthermost surgery whilst my wife, Sue, was seeing patients in the adjacent surgery. I heard her give a loud squeak and dashed through to see what had happened. An elderly gentleman was sitting with his foot up and there was a pile of odiferous dressings nearby that obviously hadn’t been changed for some time. A number of maggots were dropping off the leg onto the carpet. The patient had a large leg ulcer but it was very clean and looked as if it was healing satisfactorily. The reason … maggots ‘eat’ dead tissue but leave living tissue intact. For this reason they’ve been used for centuries for this purpose (and they work well) but squeamishness has resulted in them being largely abandoned.
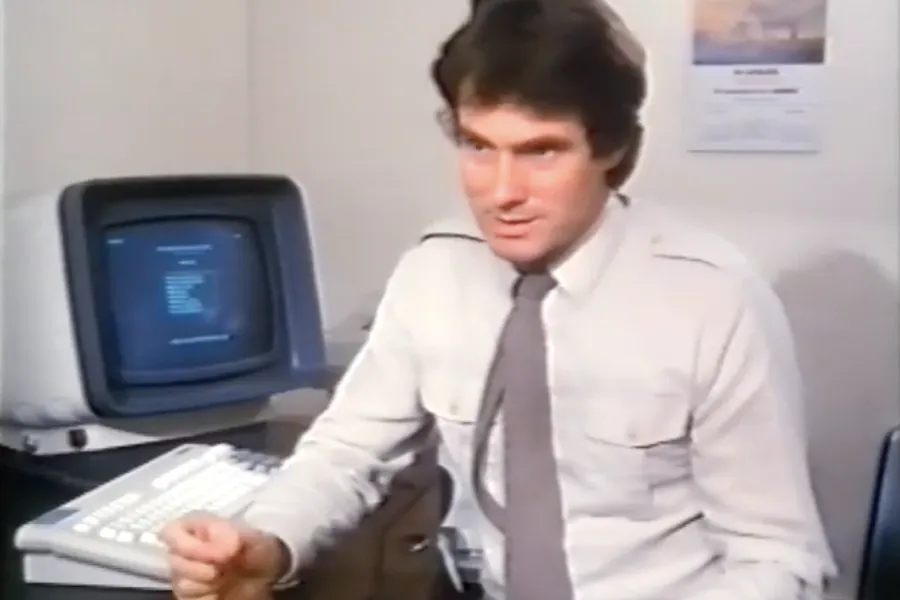
I was involved in a programme about general practice computing and, having got the bug, had one installed. It was the first proper ‘designed for GP use’ computer in an Essex practice and had a number of advantages (as seen in this short film and the photo above) and an equal number of disadvantages. It was huge but the hard drive only had something like a 2MB capacity – a tiny fraction of what a new smartphone can hold. Needless to say subsequent models were a big improvement … and now there’s one on every GPs desk.
Eventually the music shop next door (which is now the popular South Woodham Barber’s) became available so we took that over. Running a practice in two separate sites was not without its problems – but at least we had the additional space we needed. Communications were dependent on wires suspended precariously between the two buildings.
During this time we began planning the move to a purpose built surgery—of which more later.
Tune in for next week’s exciting instalment!
Dr John Cormack